From March 5-8, I attended the Advanced Technologies and Treatments for Diabetes conference in Florence Italy as a member of the press to cover the conference. My three days in Florence was spent jumping through multiple symposiums and presentations, as well as talking with various staff members from the companies represented at the conference. Here are the list of symposia I attended at the conference:
#deDoc symposium - What we wish you knew and why
Opening session - A new era in the management of T2DM and Obesity
Medtronic Symposium: Unlocking the full potential of the MiniMed 780G System
Dexcom Symposium: Leveraging CGM Early and Across the Spectrum of Type 2 Diabetes Care
Accessibility and Disparities of diabetes therapy
Medtronic Symposium: Real-world use of the MiniMed™ 780G system in the U.S.
I was also fortunate enough to get dedicated time from Medtronic Diabetes, Omnipod, Dexcom and Mannkind to discuss 1 on 1 with members of their leadership to talk about the future of diabetes care from their respective companies, you can find the interviews here:
Mannkind - Interview with Michael Castagna
While this was my first time attending ATTD, it was not my first international diabetes conference. I’ve attended ADA scientific sessions 3 times (2018, 2019, 2023) and EASD in 2022. Compared to those conferences, the venue for ATTD 2024 was very different - taking place at the Fortezza da Basso in Florence, quite literally a fortress converted into a sprawling event center campus. This made the conference a bit more spread out with a much smaller than average exhibition hall, with about an 8-9 foot ceiling compared to the extremely tall exhibit halls of the other conferences I’ve attended.
My Takeaways from ATTD: The Three A’s of ATTD:
I have decided to summarize my time at ATTD under my “Three A’s of ATTD”:
Access
Adherence
Automation
Access
My first A of ATTD is Access. In the Accessibility and Disparities of diabetes therapy symposium, featuring Partha Kar and Diabetics Doing Things Podcast alumni Dr. Ananta Adalla, there was much research shared supporting what we in the diabetes community know all too well: there are major disparities in both youth and adult populations based on race, even when you split the data by income. These disparities include:
Relationship with Providers
Perception of technology within different cultures
Inclusion and understanding of culture specifically around food
Lower adoption of tech regardless of income
Two quotes from the conference stuck out to me as thoughts that we deeply need to consider when we’re talking about diabetes access: First, Dr. Martin de Bock from New Zealand said in the Dexcom symposium: “In all countries, T2D is overrepresented in native populations and underserved populations.” Second, Dr. Partha Kar from the NHS said, that his approach to addressing disparities is very straightforward: “If you give everything to everyone, then you don’t have a disparity.”
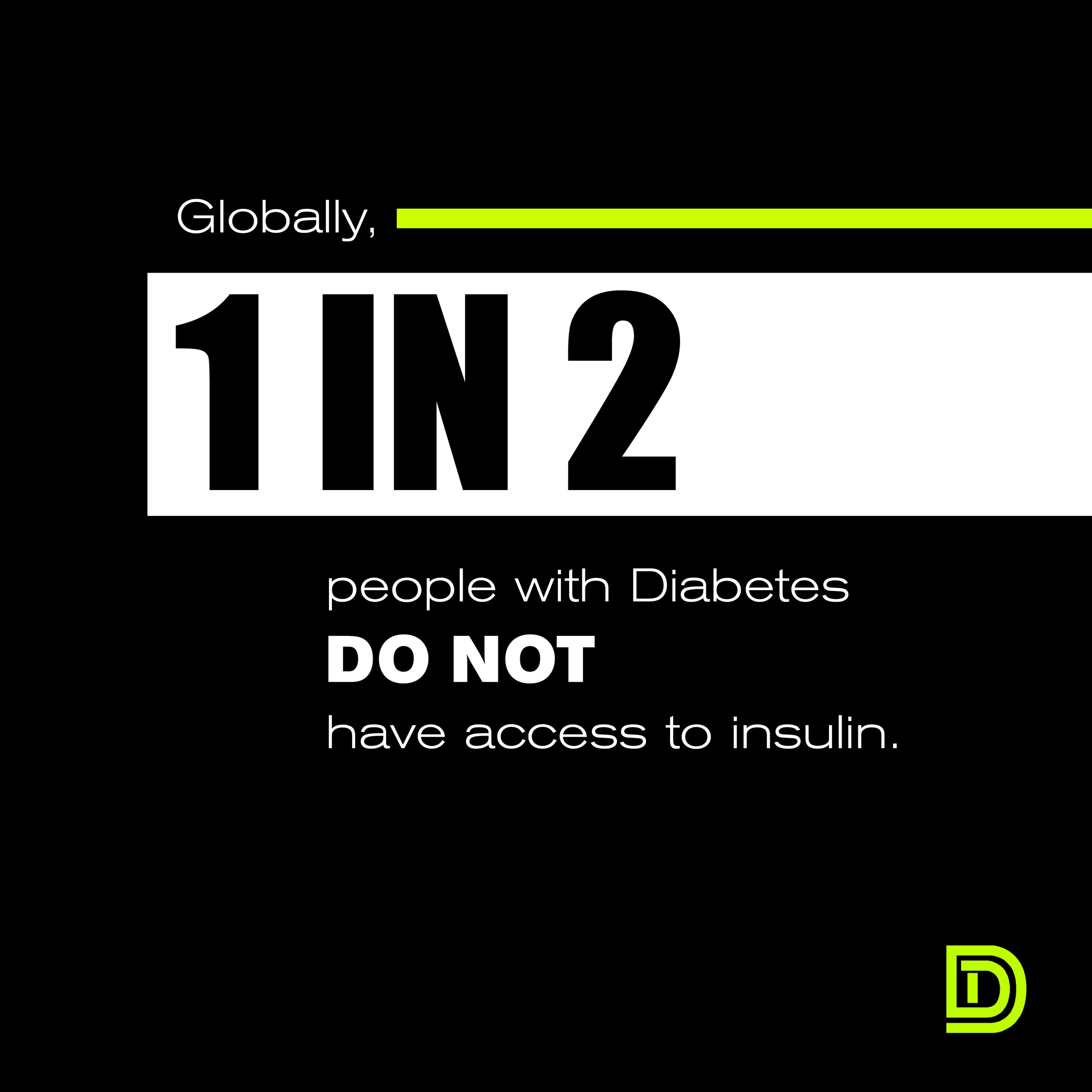
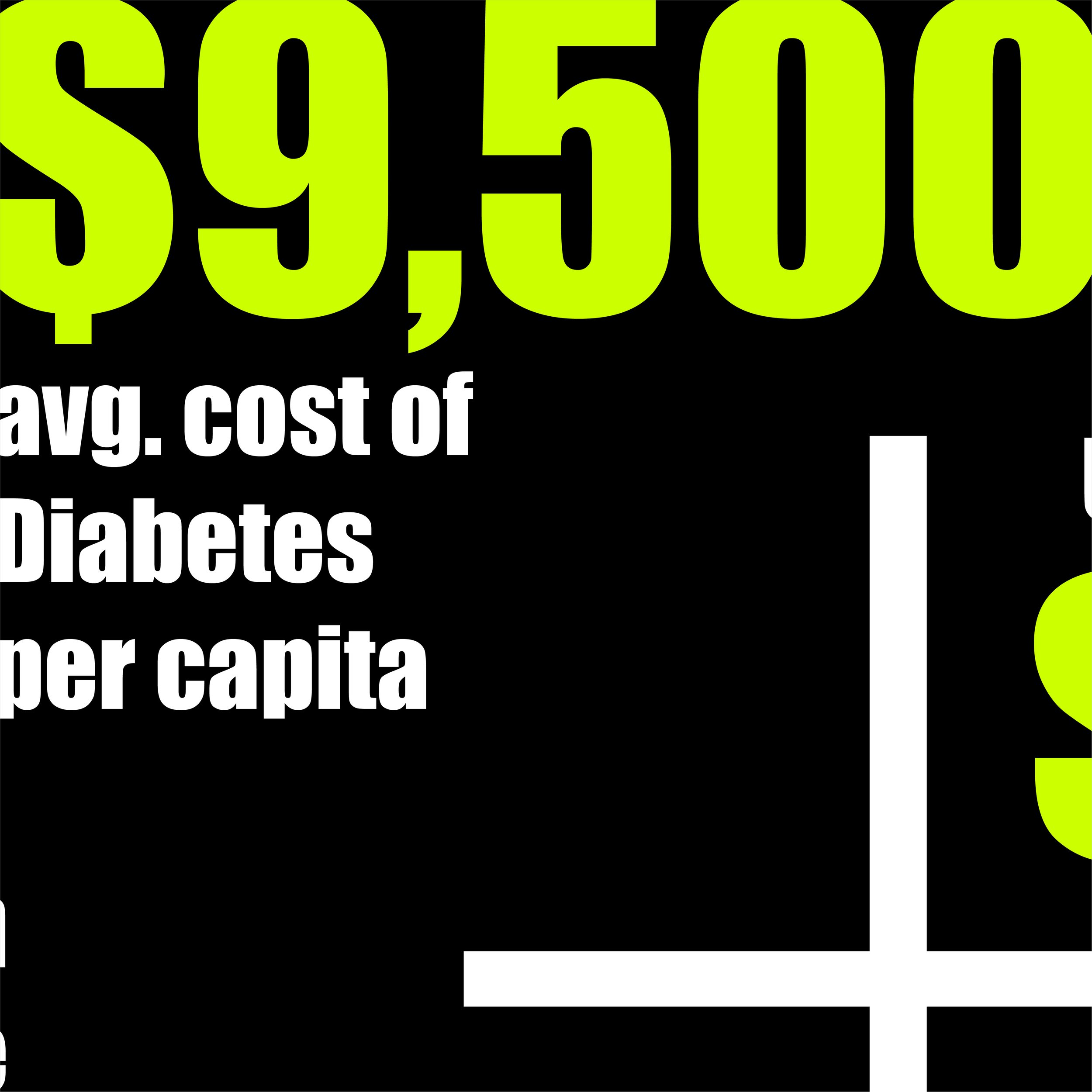
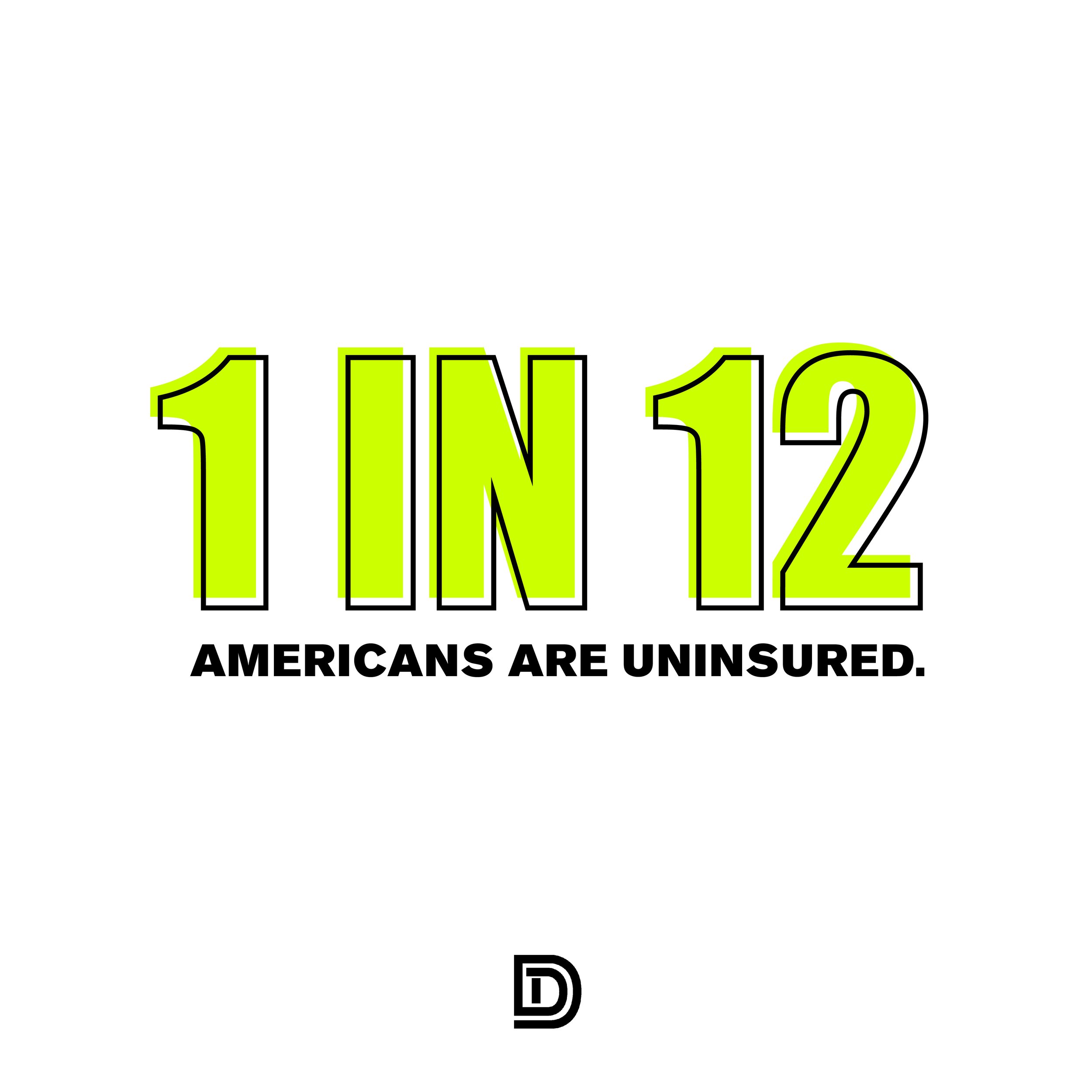
I think too often we skim over the elephant in the room regarding diabetes care and skip straight to treatments, but if patients can’t afford the coverage for the treatments or their providers don’t make them available to them, we will not be able to achieve greater outcomes across the board.
Adherence
The second A of ATTD is Adherence. This was particularly relevant for me because while Access is the number one issue, if the technology, medication or methodology doesn’t stick or isn’t sustainable, the patient will not be able to get to the benefit of improved outcomes.
In fact, the research presented by Dr. Ananta Adalla showed that CGM wear time is associated with efficacy of CGM, and with Dexcom sharing that CGM access improves outcomes across the board with Type 2 diabetes, the key to achieving these outcomes is ensuring that patience have the tools, information and support to adhere to the protocols of the therapy.
Here are some things to consider with adherence, specifically around high-risk and underserved patient populations:
You’re less likely to get a pump within a year of diagnosis if you are black/hispanic
You’re 50% less likely to have a significant diabetes complication event if you have a patient navigator/care ambassador
We have robust evidence that diabetes technology works quite well, so if there are disparities it means there are structural issues
CGM wear time is associated with efficacy of CGM
Insurance bias and racial bias are closely linked
There still exist major disparities in the use of pump & CGM in racial/ethnic minority youth
Even when income is sliced, the disparities still exist
Hesitancy to embrace technology, perceptions of device burden, embarrassment/shame, gatekeeping (felt they weren’t offered or encouraged to use tech by providers)
Relationships with providers
Differences in parent perspectives
Black Parents
Don’t want child to appear different
Feelings of defensiveness, judgement
View providers as gatekeepers
White Parents
Little concern about “otherness”
Pride in advocacy about diabetes
Providers as facilitators
Ultimately, if patient identities are not supported and empowered, adherence to technology and treatments are unlikely to be high enough to achieve improved outcomes.
Automation
My final A in the 3 A’s of ATTD is automation. There was a dramatic amount of research presented at ATTD 2024 about the impact of Automated Insulin Delivery via Hybrid Closed Loop insulin pump systems. The main systems who showed research were:
Medtronic Diabetes MiniMed 780G system
Tandem Control IQ system
Insulet Omnipod 5 system
There are also newer AID systems like Beta Bionic’s iLet ACE pump which are also coming to market, as well as DIY Loop systems like iAPS.
Ultimately, the research shows Time in Range on Automated Insulin Delivery Hybrid Closed Loop systems exceeds international consensus targets, and on the Medtronic Minimed 780G System, when the 100mg/dl glucose target and 2-hour active insulin time setting is used, 85% of users reported average Time in Range numbers greater than 70%.
While I believe devices are an extremely personal choice with many factors that vary dramatically from patient to patient, the data from ATTD 2024 unequivocally shows that AID systems significantly improve glycemic outcomes, and when referencing the DIAMOND study, Advanced Hybrid Closed Loop systems reported greater time in range and greater time in target range than CGM alone. It will be very interesting to see how this data continues to unfold as more aHCL and AID systems come to market and are able to be studied in real-world populations.
Conclusion
Overall, my time at ATTD 2024 was well-spent and while I am excited about the future of diabetes technology. It is clear that there is a dramatic need for innovation within type 1 and type 2 diabetes globally. Prevalence of T1D is increasing globally, and more adults are being diagnosed with T1D than all other age groups (LADA is the most common form of adult-onset autoimmune diabetes). The uncomfortable reality is that T1D is associated with 3-fold higher mortality, and drastically decreases life expectancy. We need to ensure that all people with diabetes, no matter the type, have access to the technology and pharmacology they need to achieve greater outcomes across the board, and the information, support and care to ensure adherence to these protocols. We are rapidly approaching a world where the standards of care for diabetes will allow people who are diagnosed T1D to receive a CGM and Automated Insulin Delivery system on the day of diagnosis, but there are real barriers to making this a reality for all.
There is also a CRITICAL need for more patient representation at these industry conferences. To have only one symposium (prior to the conference opening session) where patient stories are prominently featured (#dedoc voices symposium) is an oversight which needs to be rectified. Patient voices on issues such as Time in Target Range, Automated Insulin Delivery and Alert Fatigue can help connect providers and industry to the human stories behind these metrics.
The future of diabetes care is happening at these conferences, with or without patients, and I believe in order for us to really drive change through innovation, patients must be present.
Check out the ATTD Interview Playlist on our YouTube Channel